Pilots under the Mobile Inpatient Care @ Home (MIC@Home) Sandbox will offer convenience to patients, guide future hospital planning and create buffer for bed capacity during future pandemics
Patients now have the option of being hospitalised in the comfort of their own homes, instead of a hospital ward. Suitable patients with general medical conditions such as skin infections, urinary tract infections, or even COVID-19 can be admitted to a “virtual” ward, cared for by Mobile Inpatient Care @ Home (MIC@Home) teams. A team of doctors, nurses, pharmacists and therapists care for these patients with a combination of teleconsultations and home visits. Patients receive similar clinical care to what they would receive in hospital, such as intravenous medication and blood tests, and have 24/7 access to the care team, until they are fit for discharge. Care escalation protocols, including transfer back to hospital, could be triggered if a patient’s condition deteriorates.
Feasibility studies conducted by National University Health System (NUHS)1 and Yishun Health Medical Home between 2019 and 2021 showed that MIC@Home has been effective and safe for selected patients. Patients appreciated being able to recover in a familiar environment surrounded by their family. Based on this data, the MOH Office for Healthcare Transformation (MOHT) partnered with three MIC@Home programmes - National University Health System’s NUHS@Home, Singapore General Hospital’s SGH@Home and Yishun Health Medical Home – to scale up their implementations.
These MOHT-coordinated pilots are supported by the Ministry of Health (MOH), and implemented as part of a regulatory and financing sandbox. Under this sandbox, patients will receive programme subsidies similar to the healthcare financing coverage for a standard hospital admission.
The Sandbox was first announced in Parliament during the Ministry of Health Committee of Supply Debate in March 2022. Pilots were soft-launched in April 2022 and are set to conclude by March 2024.
MIC@Home Sandbox
The feasibility studies demonstrated that MIC@Home can be efficacious and safe for selected patient segments with low to moderate clinical acuity2. Moreover, a study conducted among patients and caregivers at Alexandra Hospital and National University Hospital from June to August 2020 showed that patient receptivity is high, despite this concept being a relatively new one in Singapore. Out of the 120 patients and caregivers surveyed, 87 respondents (72.5%) were willing to try hospitalisation at home under the MIC@Home model.
Results to date saw a number of benefits to patients, including:
- better patient-centred care:
- Most participants agreed that MIC@Home provides personalised care while maintaining patient’s quality of life, as patients were able to lead their lives in their familiar home environment while receiving treatment
- It was also thought to be convenient for patients’ and caregivers who no longer need to make multiple trips to the hospital to seek health care or visit their loved ones.
- MIC@Home could allow care providers to make clinical decisions that are better adapted to patient’s living conditions and lifestyle habits at home.
- comparable clinical outcomes:
- Length of stay and readmission rates are comparable or may be reduced. MIC@Home could also reduce hospital-acquired infections and allow patients to move freely at home without hospital restrictions, hence reducing deep vein thrombosis and functional decline in patients.
- Length of stay and readmission rates are comparable or may be reduced. MIC@Home could also reduce hospital-acquired infections and allow patients to move freely at home without hospital restrictions, hence reducing deep vein thrombosis and functional decline in patients.
- flexible hospital bed capacity:
- Hospital beds will no longer be limited to availability of physical infrastructure but will now have portable sets of equipment, which could be scaled at shorter notice.
- Hospital beds will no longer be limited to availability of physical infrastructure but will now have portable sets of equipment, which could be scaled at shorter notice.
The Sandbox aims to:
- provide care of comparable and increased resource efficiency relative to usual inpatient care, without compromising safety.
- study suitable medical conditions which could be included under the programme, and develop relevant regulatory requirements for the services.
Hospitals participating in the Sandbox will be able to trial and implement the new care model and integrate it with their existing processes. This makes it easier for subsequent service ramp-up and mainstreaming into existing practices. This model provides patient-centred and appropriate hospital care for a select group of hospital patients. It will be delivered by hospital-led clinicians and partners and augmented by telehealth and other supportive modalities of care.
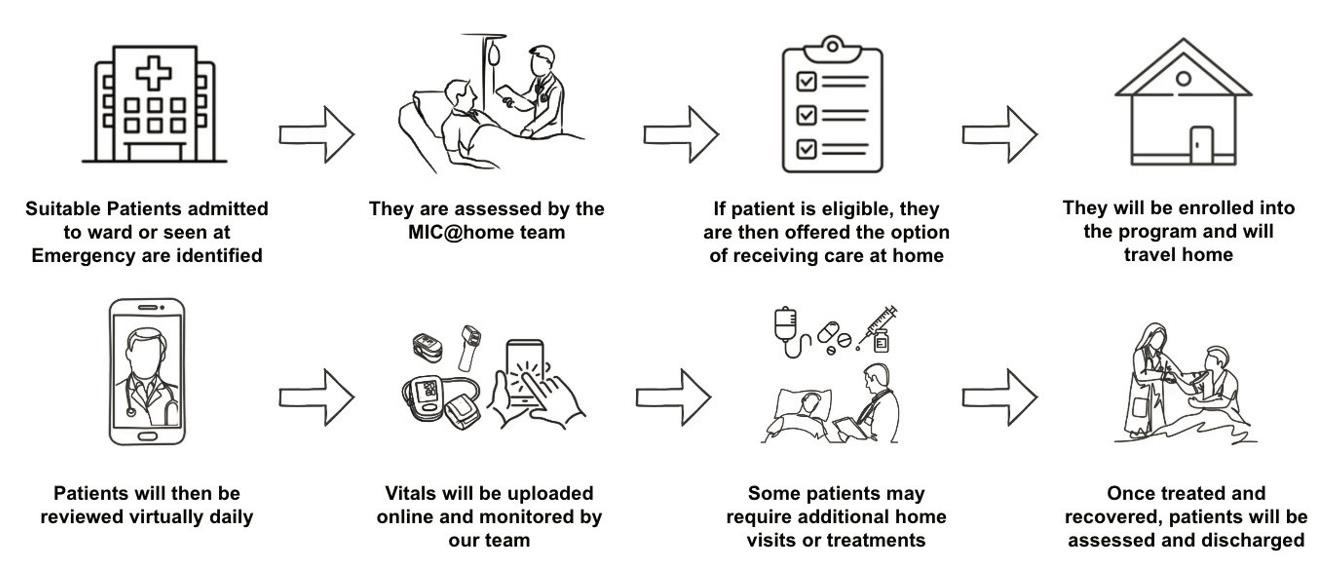
A patient’s journey through MIC@Home
Suitable patients may be referred to MIC@Home programmes from the emergency departments, hospital ward or from community nurses or doctors. The programme will be offered to patients as an alternative to being hospitalised.
A nurse meets the patient at his/her own home, setting up medication and equipment for treatment such as infusion stand and devices for teleconsultation and remote monitoring if needed. Nurses from hospitals or private partners like Speedoc, will visit the patient up to several times a day to administer drip-based medication or draw blood for testing. The care team will review patients daily either by teleconsultation or by home visits.
Physiotherapists can also visit patients at home if required. New medications are delivered to patients at home. The team is also available 24/7 for teleconsultation, should the patient encounter urgent medical issues. During care under MIC@Home, the care team will also evaluate the patient’s understanding of their own condition, medication and home environment during a visit, and also plan for follow-up post-discharge care. When a patient’s condition has improved and no longer require daily treatment, they will be discharged from the programme.
Dr Low Lian Leng, Director, Population Health and Integrated Care Office, SGH added: “We have been able to identify suitable selected patients from our emergency department and inpatient wards who can be safely managed in the home setting through a combination of in-person home visits and close virtual telehealth monitoring. Patient satisfaction is high as they can recover in a familiar home environment while the SGH team remains accessible to them. MIC@Home has helped to save bed stays for the hospital and allowed the hospital to care for sicker patients.”
Enabling recovery at home – during the COVID-19 pandemic
Prior to the COVID-19 Delta wave, KTPH, NUH, and SGH were running their proof-of-concepts pilots, supported by evaluation funding from MOHT. Thus, during the Delta and Omicron surges these hospitals were able to quickly set up their COVID Virtual Wards to serve COVID patients. This allowed about 700 COVID infected patients to safely recover at home, thus collectively saving KTPH, NUH and SGH over 5,000 bed days between September to December 2021.
Future of MIC@Home
Studies in established models in Australia3, Europe and the United States, have shown that MIC@Home models can have equivalent clinical outcomes as ward hospitalisation. Importantly, patients recovering at home report sleeping better, eating better, walking around more, and perceive their recovery to be quicker.
Healthcare professionals can build close rapport with patients over home visits and assess their conditions in their home environment. Medical care plans can also be personalised and tailored to the patient’s lifestyle and environment.
Like, SGH, the experience for NUHS and Yishun Health has been similarly positive.
Said Dr Stephanie Ko, Lead Clinician for NUHS@Home, and Consultant, Division of Advanced Internal Medicine, Department of Medicine, National University Hospital (NUH): “Our vision for NUHS@Home is to provide patients who want to be at home rather than a hospital an option to receive the care that they require. Within their home environment, patients tend to eat better, sleep better and walk around more – all of which help with their road to recovery. Our doctors and nurses can also assess patients within their home environment and better personalise treatment plans. And with the advances in technology and development of home delivery and home services, we have an opportunity to develop this way of caring for our patients.”
Dr Boh Toon Li, Lead Clinician and Principal Investigator at Yishun Health Medical Home said: “We have received positive feedback from both patients and caregivers on this service. In addition to understanding more about the patient’s medical condition, caregivers also gain knowledge and confidence to better care for their loved ones.”
Mr Lai Yi Feng, Senior Manager and Project Lead of MIC@Home at MOH Office for Healthcare Transformation (MOHT) sums it up: “As the provision of healthcare continues to shift from hospital to the home and the community, structural change and reorganisation of care delivery is pivotal. The early success of MIC@Home garnered interest to ensure its ethical, safety and regulatory standards, so that it can be recognised and scaled, as an equivalent form of inpatient care provision.”
Tech-enabling MIC@Home
Technology is a key enabler that makes MIC@Home possible. Mr Alan Goh, Assistant Chief Executive, Platform Services, Integrated Health Information Systems (IHiS), shared: “Our network of integrated systems serve as a good foundation to enable holistic care of patients. In this new pilot, we will harness a myriad of smart solutions to support the on-site and remote care for patients, including smart medical devices, apps for vital signs monitoring and teleconsultations. The solutions will include smart dashboards with decision support to the care providers, and provide alerts on anomalous health indicators. Following learnings from the pilot, IHiS will also work with our healthcare partners in forward IT planning to mainstream these services through technology.”
---
1Source: ANNALS, Academy of Medicine, Singapore. Treating acutely ill patients at home: Data from Singapore. July 28, 2022.
2In emergency and critical care medicine, clinical acuity refers to the severity of a hospitalized patient's illness and the level of attention or service he/she will need from professional staff.
3Source: New South Wales Government. Hospital in the Home (HITH). Accessed August 5, 2021.
Annex
Source: NUHS@Home
Background on NUHS@Home
NUHS@Home was started as a collaboration between the Division of Advanced Internal Medicine at the National University Hospital (NUH) and the Regional Health Service Office, admitting the first patient in September 2020. Over the last two years, the team has cared for over 150 medical patients and 1,800 patients with COVID-19 from across NUH, Ng Teng Fong General Hospital and Alexandra Hospital.
About MOH Office for Healthcare Transformation (MOHT)
MOHT is an agile unit with the mandate to address fundamental and longer-term issues critical for system-level healthcare transformation to meet Singapore’s changing demography, and health and disease patterns. MOHT works with partners to identify pilots that support its programmes and complement ongoing work at MOH and clusters/institutions, with each pilot taking a design-centric approach to implementation, involving providers, healthcare professionals, patients and caregivers at all stages of the design of solutions. MOHT adopts a value-based healthcare approach in endeavouring to achieve better health and clinical outcomes. A longer-term and broader perspective is essential in identifying key system-wide changes needed. These encompass shifts in the following three directions: (1) longitudinal, holistic care across persons’ entire life course; (2) strengthened focus on wellness and the prevention of chronic disease; and (3) empowerment of individuals and patients for better self-management.
Each collaboration will be staged with rapid build-measure-learn cycles, anchored by enablers such as technology scanning, IT, data analytics, finance and incentive redesign. From these collaborations, MOHT will develop frameworks, methodologies and toolkits to enable effective solutions to be scaled across the wider healthcare system.
For more information, visit www.moht.com.sg.
About National University Health System (NUHS)
The National University Health System (NUHS) aims to transform how illness is prevented and managed by discovering causes of disease, development of more effective treatments through collaborative multidisciplinary research and clinical trials, and creation of better technologies and care delivery systems in partnership with others who share the same values and vision.
Institutions in the NUHS Group include the National University Hospital, Ng Teng Fong General Hospital, Jurong Community Hospital and Alexandra Hospital; three National Specialty Centres - National University Cancer Institute, Singapore (NCIS), National University Heart Centre, Singapore (NUHCS) and National University Centre for Oral Health, Singapore (NUCOHS); the National University Polyclinics (NUP); Jurong Medical Centre; and three NUS health sciences schools – NUS Yong Loo Lin School of Medicine (including the Alice Lee Centre for Nursing Studies), NUS Faculty of Dentistry and NUS Saw Swee Hock School of Public Health.
With member institutions under a common governance structure, NUHS creates synergies for the advancement of health by integrating patient care, health science education and biomedical research.
As a Regional Health System, NUHS works closely with health and social care partners across Singapore to develop and implement programmes that contribute to a healthy and engaged population in the Western part of Singapore.
For more information, please visit www.nuhs.edu.sg.
About Singapore General Hospital (SGH)
Singapore General Hospital, a member of Singapore Health Services, is the public sector's flagship hospital. Established in 1821, SGH is Singapore's largest acute tertiary hospital with 1,700 beds and national referral centre offering a comprehensive range of more than 40 clinical specialties on its campus. Every year, about 1 million Singaporeans benefit from medical care delivered by its 800 specialists. As an academic healthcare institution and the bedrock of medical education. SGH plays a key role in nurturing doctors, nurses and allied health professionals, and is committed to innovative translational and clinical research in her continual strive to provide the best care and outcomes to her patients.
For more information, please visit www.sgh.com.sg.
About Yishun Health
Yishun Health (YH) is a network of medical institutions and health facilities of the National Healthcare Group in the north of Singapore. It comprises Admiralty Medical Centre, Khoo Teck Puat Hospital and Yishun Community Hospital. It also includes extensions such as Wellness Kampung.
For more information, please visit www.ktph.com.sg.
About Integrated Health Information Systems (IHiS)
IHiS is a multi-award-winning healthcare IT leader that digitises, connects, and analyses Singapore’s health ecosystem. Its ultimate aim is to improve the Singapore population’s health and health administration by integrating intelligent, highly resilient, and cost effective technologies with process and people.
IHiS played a key role in helping all major public healthcare institutions become amongst the first in Asia Pacific to achieve HIMSS EMRAM Stage 6 and 7, international benchmarks for advanced technology used in patient care.
Transforming healthcare through smart technology, IHiS has garnered more than 150 awards for its innovations. It supports more than 50,000 healthcare users in Singapore’s health ecosystem through the application of clinical informatics, computer science, data science, mechatronics, standards based IT that enables information exchange and cross boundary workflows, analysis, statistical and machine learning techniques to discover insights.
